How to Avoid Pitfalls in License Verification


Any accredited healthcare organization can tell you that proper licensing is essential for their facility to run properly. Hiring unlicensed or sanctioned professionals can severely damage your business’s reputation — and put your patients’ safety at risk.
Here are a few do’s and don’ts to help you avoid common pitfalls in license verification.
What to Do:
Follow Accreditation Standards
Accreditation is more than just good practice for your organization — it’s federal law. Your organization must keep up with the license verification rules and standards set by organizations like The Joint Commission. These standards are designed to mitigate the risk of fraudulent licenses and credentials, so keeping compliance is really in your best interests.
Make sure that your facility (particularly your HR department and hiring managers) is up to date on all accreditation and license verification standards, and regularly review these standards to keep them at the forefront of your minds.
Perform Ongoing License Monitoring
A healthcare professional may be accredited when you hire them, but that can change at any time. For this reason, it is essential to continue to monitor your physicians, nurses, and other employees to confirm that their licenses are in good standing.
One easy way to do this is through a human resource information system, or HRIS. These programs can track data automatically, checking for expired licenses, sanctions, and other potential problems with just the click of a mouse. Your team can receive alerts when an employee’s license becomes invalid or questionable, thereby removing the risk that an unlicensed individual can slip through the cracks.
Use Primary Source Verification
Unfortunately, it can be easy for bad actors to submit fraudulent or expired credentials during the hiring process. This is why it’s important to do additional digging — and the best way to do this is through primary source verification.
Primary source verification is… well, exactly what it sounds like. During the verification process, you should reach out to the original accrediting body, like the state or federal agency that regulates licenses. You can follow up this verification by checking databases like the American Medical Association (AMA) Masterfile, but this initial primary source verification is essential to be compliant.
Examine Peer Reviews
All credentialed healthcare professionals must have documentation indicating that their license has undergone peer review. It’s important to examine these reviews to verify credentials and licenses, as they can reveal potential incompetence of the prospective hire.
Make sure to thoroughly examine peer reviews during the verification process. If you fail to do so, you might miss some key information that could shift your view of the candidate.
Utilize the Expertise of a Third-Party License Verification Organization
Sometimes, it can be difficult to conduct a truly thorough verification process. Most healthcare facilities are very busy, with every employee stretched to their limit on a regular basis.
However, this doesn’t mean that you should forego verification. Instead, you can work with a third-party who is dedicated to helping you through the verification process. At ComplianceLine, we can either do the verification for you or equip you with automated software that will handle the verification behind the scenes while you do your daily activities.
What Not to Do:
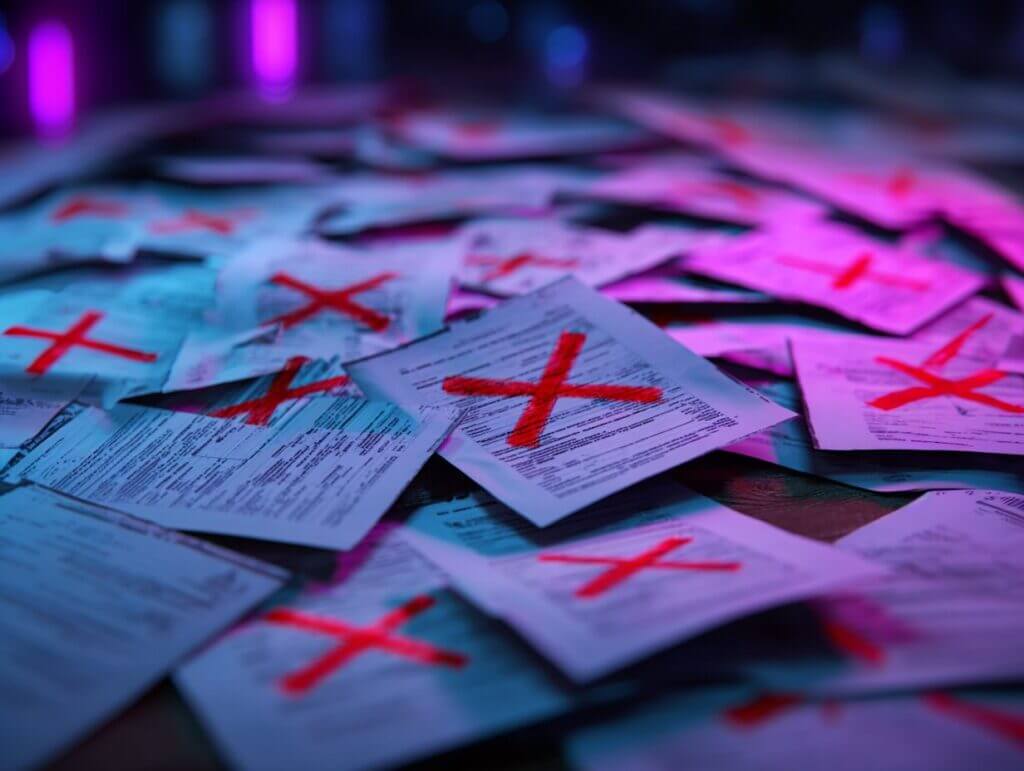
Accept Applications with Incomplete Information
If a candidate has left something off of their application, you usually don’t want to know the reason why. Either they don’t have the credential or experience you’re looking for, or they did have it and have let their license lapse or lost their accreditation. If you notice incomplete portions on an application, it’s best to move forward cautiously.
Ignore Pending Lawsuits or Settlements
Pending lawsuits or settlements can tell you a lot about a candidate in his or her worst moments. In order to properly vet your prospective hires, you will need to thoroughly research any litigation in which they’ve been involved. Talk to their medical liability provider. Review the details of the case. These details can help you make a more informed decision about the candidate’s ability to safely treat your patients.
Neglect to Contact References
Most job applications today require the candidate to provide references. For some industries this might seem like a formality, but in the world of healthcare it is absolutely critical. You must get in touch with these references and ask them thorough questions about your prospective hire — and make sure your candidate includes multiple ways to contact each reference in order to facilitate this process.
Fail to Allot the Proper Time
Credentialing can be a very time-consuming process. Unfortunately, this can be a problem, as time is of the essence in healthcare. It is important to begin your hiring process with ample time to conduct a thorough verification.
Make sure that you plan at least 45-90 days for the verification process — or, if you want to shorten that time, then have a third-party vendor help you complete the verification while you vet your candidate.
Protection Against Unlicensed Professionals
If you follow these do’s and don’ts, you will protect your organization and your patients from unlicensed medical professionals. And if you work with a vendor like ComplianceLine, you’ll be able to complete the verification process quickly and easily.