NCQA’s 2025 Credentialing Guideline Updates: A Compliance Officer’s Guide


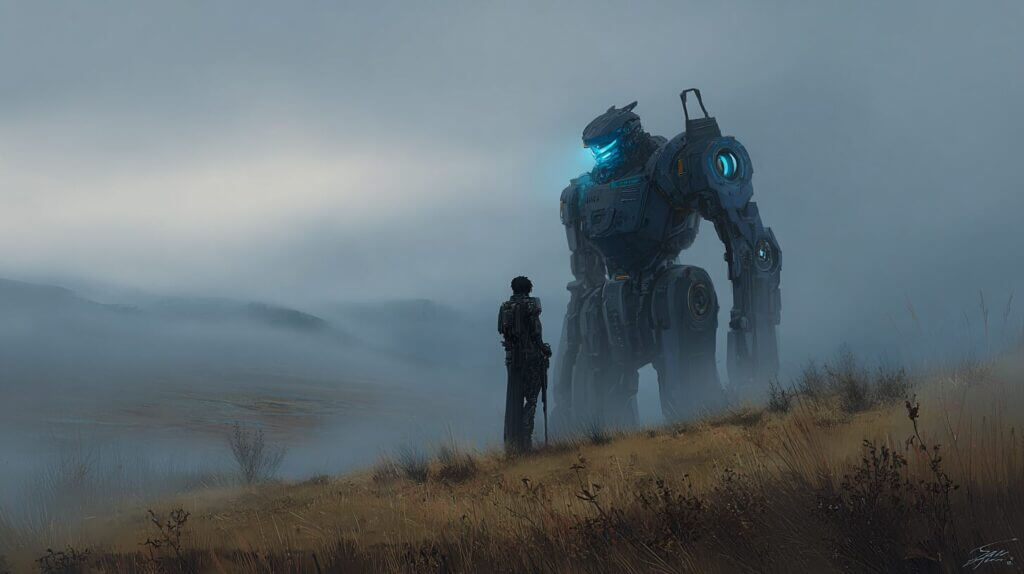
Learn About ecoCheck
LEARN MOREThe National Committee for Quality Assurance (NCQA) has introduced significant updates to its credentialing standards, effective July 1, 2025, marking a transformative shift in healthcare quality management. These changes primarily focus on accelerating verification timelines, enhancing monitoring requirements, and leveraging technological solutions for improved oversight.
The National Committee for Quality Assurance’s (NCQA) 2025 credentialing standards represent a significant shift in healthcare quality management, emphasizing automation, enhanced monitoring, and data-driven oversight. These updates reflect the industry’s evolution from paper-based systems to digital solutions, with a focus on patient safety, provider accountability, and streamlined verification processes. The following blog explores the major changes and their implications for healthcare organizations.
Modernized Verification Timelines
- The transition from traditional paper-based verification to automated systems has prompted NCQA to reduce verification windows significantly.
- Healthcare organizations must now complete credentialing verification within 120 days for NCQA-accredited organizations and 90 days for NCQA-certified organizations, compared to the previous 180-day and 120-day windows respectively.
- This change acknowledges that modern technology enables faster, more efficient verification processes while ensuring data accuracy and compliance.
Enhanced Monitoring Requirements
- NCQA has implemented mandatory monthly monitoring requirements for all enrolled providers, marking a significant shift in ongoing oversight responsibilities.
- Organizations must now conduct comprehensive checks every 30 days for Medicare and Medicaid exclusions, sanctions, and disciplinary actions, while also incorporating SAM.gov as a primary verification source.
- This systematic approach ensures continuous visibility into provider eligibility and helps organizations maintain high standards of patient safety throughout the credentialing cycle.
Integration of License Expiration Tracking
- The new standards mandate monthly tracking of license expiration dates for all credentialed providers, representing a fundamental change in credential management.
- Healthcare organizations must develop robust systems to monitor expiration dates continuously, shifting from the traditional three-year credentialing cycle to a more dynamic, ongoing monitoring process that ensures providers maintain active licensure at all times.
Emphasis on Data Integrity and Reporting
- NCQA’s updated guidelines place heightened importance on comprehensive self-serve reporting capabilities and audit logs.
- Organizations must maintain detailed records of data changes, monitoring gaps, and verification activities, demonstrating a commitment to transparency and accountability in credentialing processes.
- This requirement necessitates sophisticated technological infrastructure to track and report credentialing activities effectively.
Social Demographic Data Collection
- The standards now encourage the collection of provider demographic data, including race, ethnicity, and languages spoken.
- While completion remains voluntary, this initiative represents NCQA’s commitment to promoting health equity and enabling healthcare organizations to better serve diverse patient populations through improved provider-patient matching and cultural competency.
Infrastructure and Technology Requirements
- Healthcare organizations must invest in robust technological solutions to meet the new standards effectively.
- The requirements necessitate automated systems capable of handling continuous monitoring, reporting, and verification processes, marking a shift away from manual credentialing methods toward more sophisticated, integrated solutions.
Compliance Timeline and Implementation
- Organizations now must comply with these changes, which took effect July 1, 2025, and ensure their systems meet the new standards.
- The implementation timeline requires careful planning, resource allocation, and potential technological upgrades to ensure compliance with all new requirements while maintaining efficient operations.
Accountability and Patient Safety
- The new standards emphasize the critical role of credentialing in patient safety and quality care.
- Organizations must establish clear protocols for addressing adverse findings during monitoring, including reporting mechanisms to appropriate committees and taking prompt action when issues are identified.
Closing Summary
These comprehensive updates to NCQA’s credentialing standards represent a significant evolution in healthcare quality management, emphasizing the importance of continuous monitoring, technological integration, and data-driven decision-making. Organizations must adapt their processes and infrastructure to meet these enhanced requirements, ultimately promoting improved patient safety and healthcare quality. Success in implementing these changes will require careful planning, resource allocation, and a commitment to ongoing improvement in credentialing practices.